With the slow rollout of COVID-19 vaccines, ’vaccine nationalism’ is only slightly more rife than the calls against it. The focus on ‘vaccine nationalism’ by critical thinkers and activists around the world misses some key lessons of the pandemic elaborated in my October 2020 article, ‘Access to medical supplies and devices — the lesser known story of COVID-19 and medical monopoly.’ This piece summarises my October 2020 piece and links it to new developments, most importantly — amid the deadly third wave — the need to organize for a ZERO-COVID approach to end the pandemic.
COVID-19 and Medical Monopoly
As with N-95 masks and ventilators, the underproduction of vaccines is at the root of vaccine shortages and so-called vaccine nationalism, both of which are systemic to monopoly capital.
In the first wave of the COVID-19 pandemic, news of medical technology shortages surfaced: from N95 respirators to protect healthcare workers from contracting and spreading the novel coronavirus, to COVID-19 testing materials, to ventilators for infected patients unable to breathe.
A well publicised example globally was the shortage of personal protective equipment (PPE). From March 2020, workers in rich as well as impoverished countries were demanding employers to provide N95 respirators, gowns and gloves.
In the United Kingdom, when not on duty, public hospital workers demonstrated for PPE throughout March and April. By the end of April, the Guardian had recorded over 100 COVID-19 deaths of healthcare workers in the UK.
Also in April, as Canada’s largest privatised elder care sector was becoming a hotbed of the pandemic, the country’s largest nurses’ union, The Ontario Nurses’ Association, had to file a court petition to push private long term care homes to provide protective gear to nurses and other healthcare workers.
In Northern Italy mid-March, during the height of the first wave there, factory workers staged wildcat strikes demanding protective gear. While most shops and public places in Italy were closed under lockdown by March, factories remained open and without income supports, factory workers were forced to continue working.
In late April and May, in public as well as private hospitals in the Eastern Cape, South Africa, reproducing typical hospital hierarchies, management and doctors were hoarding PPE. Nurses and other healthcare workers contracted the virus in large numbers. Similarly in the Peruvian Amazon city of Iquitos, 80 per cent of hospital workers lacking PPE tested positive for COVID-19 by mid-May.
The battle for PPE continues for a range of workers globally as vaccines remain in short supply and the virus resurges and mutates.
Another example that received far less media coverage, particularly in rich countries, is the shortage of COVID-19 testing materials. As early as March 2020, the World Health Organisation (WHO) was admitting the emergence of a global shortage of chemical reagents needed to process COVID-19 PCR tests.
In early June, during a crucial period for testing and contact tracing in South Africa, the Minister of Health acknowledged that both public and private labs were slow in processing tests due to a shortage of test kits and accompanying reagents. By early July, private pharmacy group, DisChem, closed its testing facilities citing delays in receiving test results as the reason.
Speaking of the African continent as a whole, the Minister of Health of the Central African Republic, Pierre Somse, stated in mid-July “we are in a scarcity, a misery of tests,” attributing the Africa-wide lack of testing materials to a shortage of global solidarity.
A scientific study published February 17, 2021 online argues that the spread and impact of COVID-19 are likely far greater in Africa than what has been understood. Based on post-mortem analysis of 372 deceased people in the University Teaching Hospital morgue, Zambia’s largest hospital, between June and September 2020, the study shows that most COVID-19 related deaths were in the community, where testing is not occurring, and few people who died at healthcare facilities were tested, despite presenting with symptoms typical of Covid-19.
Explaining medical technology shortages
High demand and in turn, local and global shortages, is the most commonly provided explanation for the chronic lack of PPE, testing reagents, vaccines and other COVID-19 related medical technology. At best, governments are blamed for epidemic unpreparedness and not assuring the stockpiling of supplies despite long standing studies and recommendations from previous epidemics.
As I show in Rethinking Unequal Exchange, however, the problem runs much deeper. The medical device and diagnostics industry — like the better known story of pharmaceuticals — is a monopoly, with all the attendant features of for-profit production dominated by a small few.
The makings of monopoly
In the instance of medical devices and diagnostics, the process unfolded from the late 19th century onward, largely in the USA. The process included creating first local, then global markets for new medical commodities, patenting to maximise the price of these commodities by limiting production and supply, and controlling the direction and scale of technological innovation through the acquisition of firms with ideas that were investing in innovation.
Using such manoeuvres, US-based companies have played a major role in establishing and leading the multinational medical device and diagnostics industry. Incorporating countries around the world, this history is part of what Giovanni Arrighi has termed US world hegemony. Where other major medical technology firms emerged, for instance in Western Europe, it necessarily involved the use of similar manoeuvres.
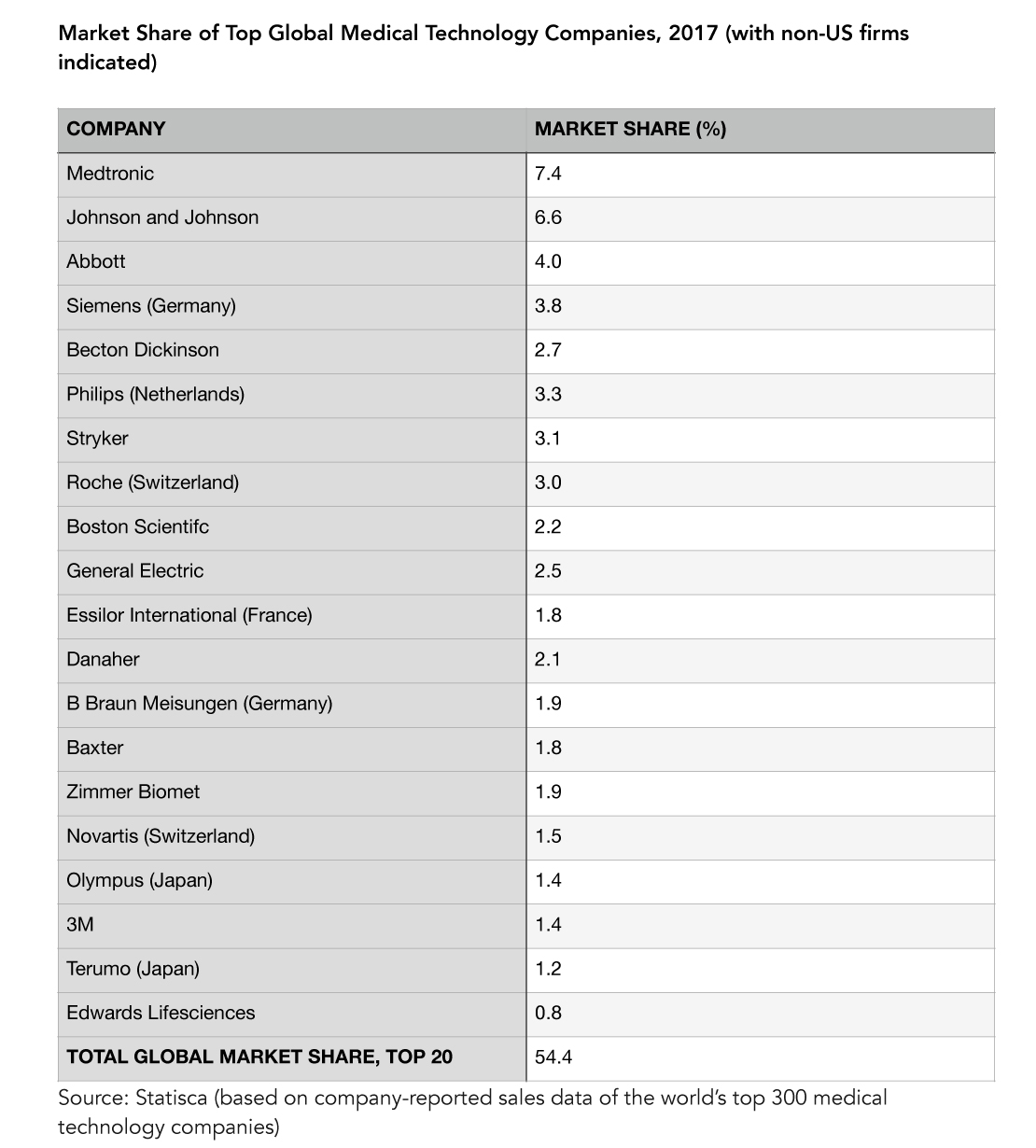
Over time, some companies fared better than most. By 1999, 12 percent of firms came to dominate the US medical technology industry. More specifically, 733 of 5,998 companies accounted for 80 per cent of industry sales, with the top 2 per cent accounting for 48 per cent of these. Today, the total number of companies in the industry has gone down to 1,083, suggesting deepening monopoly control. Along the same lines, according to a 2017 estimate, the top 20 medical technology companies controlled just under 55 per cent of the global medical technology market, the majority of which were US American firms.
Further suggesting deepening monopoly control are the numbers of US medical technology firms figuring in Fortune Magazine’s listings of top performing companies in the USA (Fortune 500) and internationally (Global 500) between 2005 and 2019. In 2005, 7 US medical technology companies (Baxter, Becton Dickinson, Boston Scientific, Medtronic, Guidant, Stryker and Danaher) figured in the Fortune 500, and 1 US medical technology company (Abbott) featured in the Global 500. By 2019, 5 of these companies (Baxter, Becton Dickinson, Boston Scientific, Stryker, Danaher) figured in the Fortune 500, and 2 (Medtronic, Abbott) featured in the Global 500. Meanwhile, the market size of the US medical technology industry increased from 67.9 billion USD in 1999, to 169.3 billion USD in 2018 and 425.5 billion USD globally. Two significant acquisitions occurred in this period. In 2006, Boston Scientific’s acquired Guidant, for 27 billion USD, or just under 40 per cent of the industry’s total market value in 1999. In 2015, Zimmer acquired Biomet, thus gaining a place in the Fortune 500. By 2019, Zimmer ranked 387, climbing from 431 in 2016.
Impact on hospitals
Through the 1980s, monopoly production of medical technology was the primary cause of cost escalation for US hospitals, the major consumers of medical devices and diagnostics. Monopoly priced medical technology can be traced over time as a major cost pusher in public healthcare systems as well, for instance in Canada.
Along with reductions in public financing, medical technology induced cost escalation lead to the failure of 550 community hospitals in the USA, and mergers of several hundreds. Around the same time, the number of corporate-owned hospitals in the USA more than doubled, increasing from 445 in 1978 to 955 in 1984.
As hospital care became commodified in the USA, it quickly took on a monopoly structure like that of medical technology. Three companies — Hospital Corporation of America, Humana, and American Medical International — came to own just under three quarters of the 35.1 per cent of the country’s hospital beds controlled by the private sector.
By the mid-1990s, two of these companies — after American Medical Holdings took over American Medical International — began ranking in the Fortune 500. This marked the beginning of multi-hospital systems becoming a high profit industry in the USA. Between 1996 and 2020, Humana rose steadily from 279th place in Fortune’s top 500 US companies, to 52nd.
Impact on nurses
In order to maintain high profitability, particularly given the monopoly-driven high costs of medical technology, the hospital industry looked to reduce labour costs through the 1990s. Nursing work and compensation were restructured, undoing the gains made by nurses with regard to professional autonomy and compensation. Part of the cost saving shift was the increased use of internationally trained nurses entering the US on temporary work permits and employed at inferior levels of wages and working conditions to local nurses. Reduced professional autonomy, worsening working conditions and the overall devaluing of nursing labour have been key causes of the dwindling supply of nurses in the USA and elsewhere.
Full circle to COVID-19
The COVID-19 pandemic has amplified the gravity of the global nurse shortage. In the attempt to make up for the shortfall of nurses, Rwanda, for instance, has turned to using robots for COVID-19 screening and delivery of care. These robots, another form of medical technology, are not produced in Rwanda and come at a monopoly price that is unlikely to be sustainable.
Testing reagents, N95 respirators, and ventilators are technologies that are far more crucial than robots to manage COVID-19. All are produced by companies in Fortune’s current top US 500 or/and Fortune’s Global 500 rankings — some since the 1990s, some since the early 2000s, and one since 2017.
Becton Dickinson and Danaher (the parent company of Cepheid) — ranking 187th and 161st respectively in the US top 500 — produce reagents that are necessary to process COVID-19 tests. Danaher/Cepheid reagents are designed to function only with Danaher/Cepheid diagnostic machines. Mixing and matching is not part of the design. Nor are the machines compatible with reagents made using a method provided by the World Health Organisation before Cepheid created COVID-19 tests. Becton Dickinson uses the same strategy of market control.
Though South Africa was among the first to procure Cepheid’s GeneXpert Systems diagnostic machines, it has not been able to access adequate supplies of reagents. Many blame state failure alone for delays in testing and contact tracing. Monopoly control of testing technology, however, is much more plausible as the major explanation for why South Africa — despite imposing one of the strictest, most extensive lockdowns globally — was not able to diagnose COVID-19 cases quickly enough to conduct contact tracing and stem the spread of the virus in the first wave. The high number of excess deaths, or deaths exceeding historical seasonal averages and unaccounted for as COVID deaths — 143,543 for the period 3 May, 2020 to 24 February, 2021 — can also be largely explained by the lack of testing and testing technology.
Similarly, Peru conducted extensive testing early in the first wave of the pandemic but faced difficulty accessing reagents to process the tests. During the first wave, Peru surpassed the USA in terms of confirmed cases per 1 million population (as of early October 2020, 9,378 and 9,286 respectively). Thailand is another example. In Bangkok, three hospitals suspended testing as early as March 2020 because they had run out of reagents. Thailand then ramped up prevention through mass education as the major thrust of its COVID-19 strategy — more on this below.
The company 3M — ranking 103rd in the Fortune 500 — is the world’s largest producer of N95 respirators. In early April, Kentucky state Governor Beshear called on 3M to release the patent on the N95 respirator so that other companies could produce them. Shortly after, President Trump invoked the Defense Production Act to among other things, stop 3M from exporting N95 respirators and other medical devices. Later on that month, next door in Canada, trade union and other activists called for a General Motors plant sitting idle for a year to be reopened to produce N95 respirators. Though the plant was reopened to produce masks, it was not the N95 respirators. This was undoubtedly due to the 3M patent.
Rather than releasing the patent, 3M CEO was quite public as early as March about the company’s priority: working with large e-marketplace operators to identify and report counterfeiters and price gougers of N95 respirators and other 3M medical devices. By mid-July, 3M had filed 18 lawsuits after tracing 4,000 reports globally of fraud, counterfeiting and price gouging of its products.
Medtronic, an Ireland-based medical technology company produces ventilators and technologies to treat some 40 medical conditions. It has featured in Fortune’s Global 500 since 2017. With the rise of COVID-19, along with the creation of virtual training in the use of its ventilators, the company has opened a ‘COVID-19 path for idea submissions’ online. Medtronic’s focus is securing further monopoly profit and control through pandemic-related training and innovation.
One big solution – Mobilize Organize!
Swati Thiyagarajan and others have argued that the extent of human incursion and destruction of the earth has exposed us to viruses with which we would otherwise not have had to interact. These viruses are powerful and able to transform themselves quicker than the conquering spirit of biomedical science. Focusing on vaccines as the primary means of preventing the spread of the novel coronavirus leaves countless people exposed to new, yet more destructive strains of the virus that are conceived while the excluded wait passively for vaccine roll-outs.
A people centred, Zero-COVID strategy is the alternative around which it is crucial to mobilise in the short term. Such an approach to prevention challenges people to work together to eradicate the virus in their geographic spaces with the aid of popular education, grassroots target setting, decommodified testing technologies, tracing, and limited but strategic lockdowns that include income supports and nutritious food delivery to homes. The Zero-COVID strategy has been used successfully in places like Cuba, Vietnam and New Zealand.
If activists around the world fail to push for a Zero-COVID strategy in their local and national spaces, we risk seeing several more waves and new strains of COVID-19, further burnout of nurses and other health workers, and deeper stratification of the global health labour force already concentrated in richer countries.
In the medium term, only by rallying against commodified healthcare can the underproduction of vaccines, N-95 masks and other medical technology be brought to an end.
The commodification of healthcare is a reality in most countries. Rallying against it in national and subnational spaces is a path to organising globally against world capitalism that has been opened by the pandemic unlike any health issue has done previously.
As I have discussed in an article on Interferon 2b and Cuba’s other treatments for COVID-19, decommodified universal healthcare is the alternative to monopoly-driven healthcare ravaging countries around the globe. Not for profit production and delivery of all health related goods responding to general and specific human needs of the majority of any given country is the only means to assure quality health for all, in pandemic as well as non-pandemic times.
More concretely, decommodified universal healthcare is ecologically sound, public sector production of everything from food to psychological support, medicines to medical technology, and medical care. Rather than results based management and other corporate models adopted by most state owned enterprises globally in the past four decades, such public production would be designed and managed democratically by citizens, health professionals, scientists, and the range of other workers involved.
Taxation of corporations and rich individuals would be the primary means of financing decommodified universal healthcare. Due to the social importance of health related goods, and high employment potential given the extent of need in most countries around the globe, decommodified universal healthcare would constitute a significant segment of needs based, ecologically sound, nationally focused economies.
Decommodified universal healthcare contrasts with the narrow notion of universal health coverage in the United Nations Sustainable Development Goals (SDGs). SDG-3 pertains to health and embodies results based management, favouring public procurement of healthcare commodities produced for profit. In order to do this, the UN and other intergovernmental bodies encourage impoverished countries to accumulate further debt through loans from the International Partnership for Health. Rather than this, these global bodies should be supporting healthcare financing through general taxation by devising strategies to retrieve the trillions of dollars of wealth lost to the global majority through tax avoidance by rich individuals and corporations like those discussed here.
Amid disintegrating human as well as ecological health and a collapsing world economy, ZERO-COVID now, decommodified universal healthcare in the medium term, and needs based, nationally focused, ecologically sound production are central to rebuilding world society.
This article was first published in The Bullet: https://socialistproject.ca/2021/03/fighting-medical-monopoly/
Salimah Valiani is a poet, activist, and researcher. Born in Calgary, Alberta, Canada, of a Ugandan mother and Tanzanian father, like her parents, Salimah left home in her late teenage years and began a journey of study and work that included extended stays in Montreal, Quebec; London (UK); New York City and Binghamton (USA); Toronto and Ottawa, Ontario; and Cape Town, South Africa. She has published four collections of poetry: breathing for breadth (2005); Letter Out: Letter In (2009); land of the sky (2016); and Cradles (2017). Her latest publication is the poem-story,” Dear South Africa,” one of seven pieces in Praxis Magazine’s 2019-2020 Chapbook Series. Salimah’s new poetry collection, 29 leads to love, will be published by Inanna Publications in 2021. Check out her work online at: https://www.facebook.com/SalimahValianiPoet.

Excellent expose on the monopolistic dominance by pharma that perpetuates Covid-19 and in general, healthcare systems around the world. This is a wake up call. Thank you, Salimah for your research and your activism.